What’s different?
4 Distinctives of Christ-Centered Healthcare
As I travel visiting clinics, students and with folks who hope to start a Christian healthcare ministry, I am often asked, “What distinguishes a Christian clinic from a non-faith-based clinic?” Usually, I respond by asking what they would expect from a Christian clinic. And people typically talk about excellence, compassion, and affordability. Certainly, any clinic that seeks to represent Christ must strive for those qualities. But all clinics, faith-based or not, should be excellent and compassionate. Those are universal qualities, not qualities that are “uniquely Christian”.
All Christian clinics should exemplify excellence and welcoming customer service. But having personally visited a ton of Christian clinics, I want to suggest four areas where we should be unique if we strive to fully embrace what it means to be a Christ-centered clinic. They are restoring patient dignity, organizational culture, embracing a prophetic role, and investing in a ministry focus beyond your organization’s immediate interest.
Click here to read the full essay by Steve Noblett, Chief Executive Officer of Christian Community Health Fellowship.
Vitamin D Deficiency
Lack may increase risks
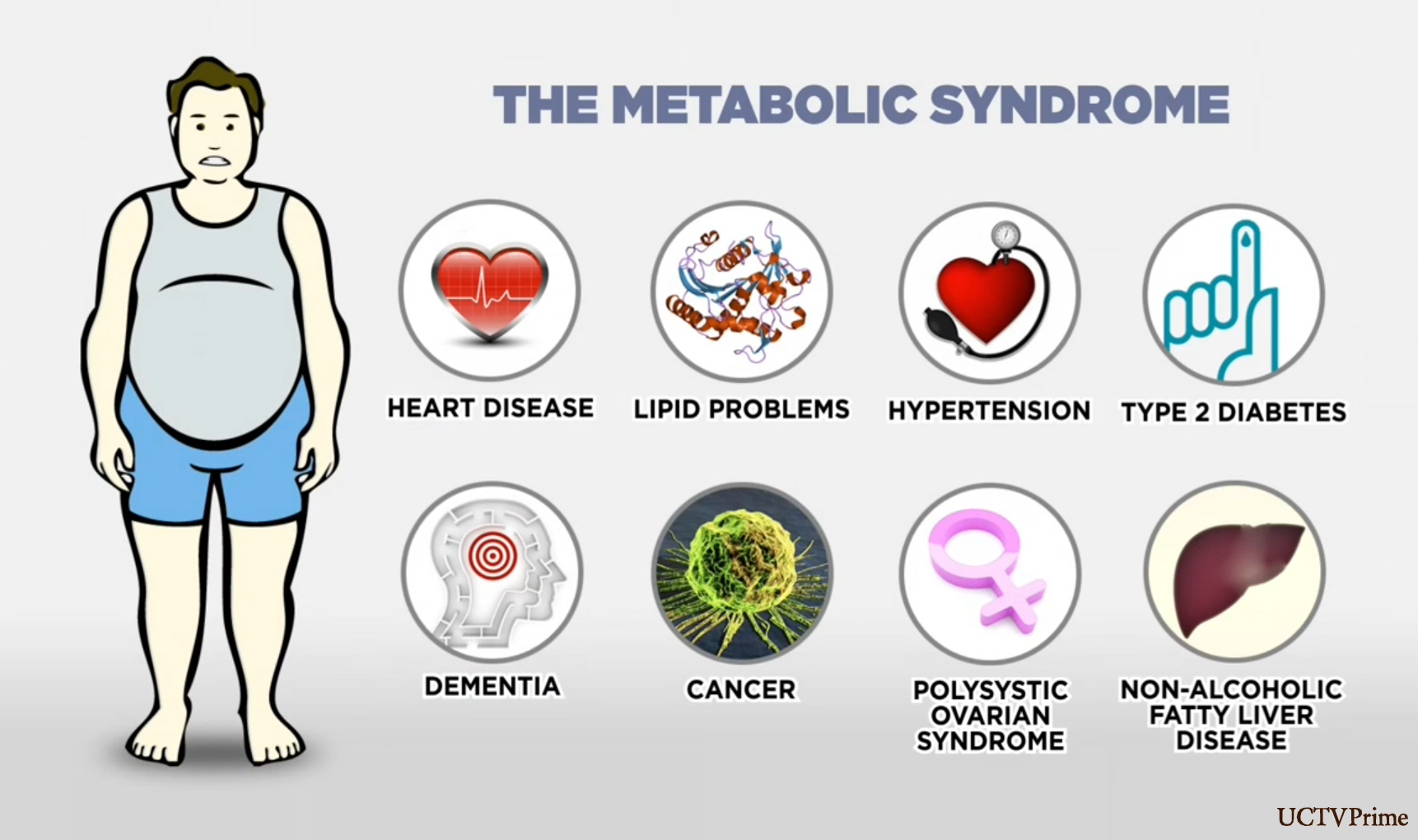
According to a new study, Vitamin D deficiency may increase the risk for metabolic syndrome* after menopause.
Researchers looked at 463 postmenopausal women with cardiovascular disease who weren’t taking vitamin D supplements. More than two thirds of the women had vitamin D levels lower than 30, which was considered insufficient. Of these women, 58% had metabolic syndrome, compared with 40% of women with sufficient vitamin D. When the vitamin D level was below 20, the odds of metabolic syndrome were doubled.
This observational design can’t prove causation, and more studies are needed. But because metabolic syndrome is a major risk factor for CVD, maintaining adequate vitamin D levels in postmenopausal women may be an important preventive measure.
Charles Vega, MD, clinical professor of family medicine at the University of California at Irvine.
*Metabolic syndrome is a very common and dangerous complex of disorders noted primarily in overweight individuals who develop high blood pressure, diabetes and elevated cholesterol levels.
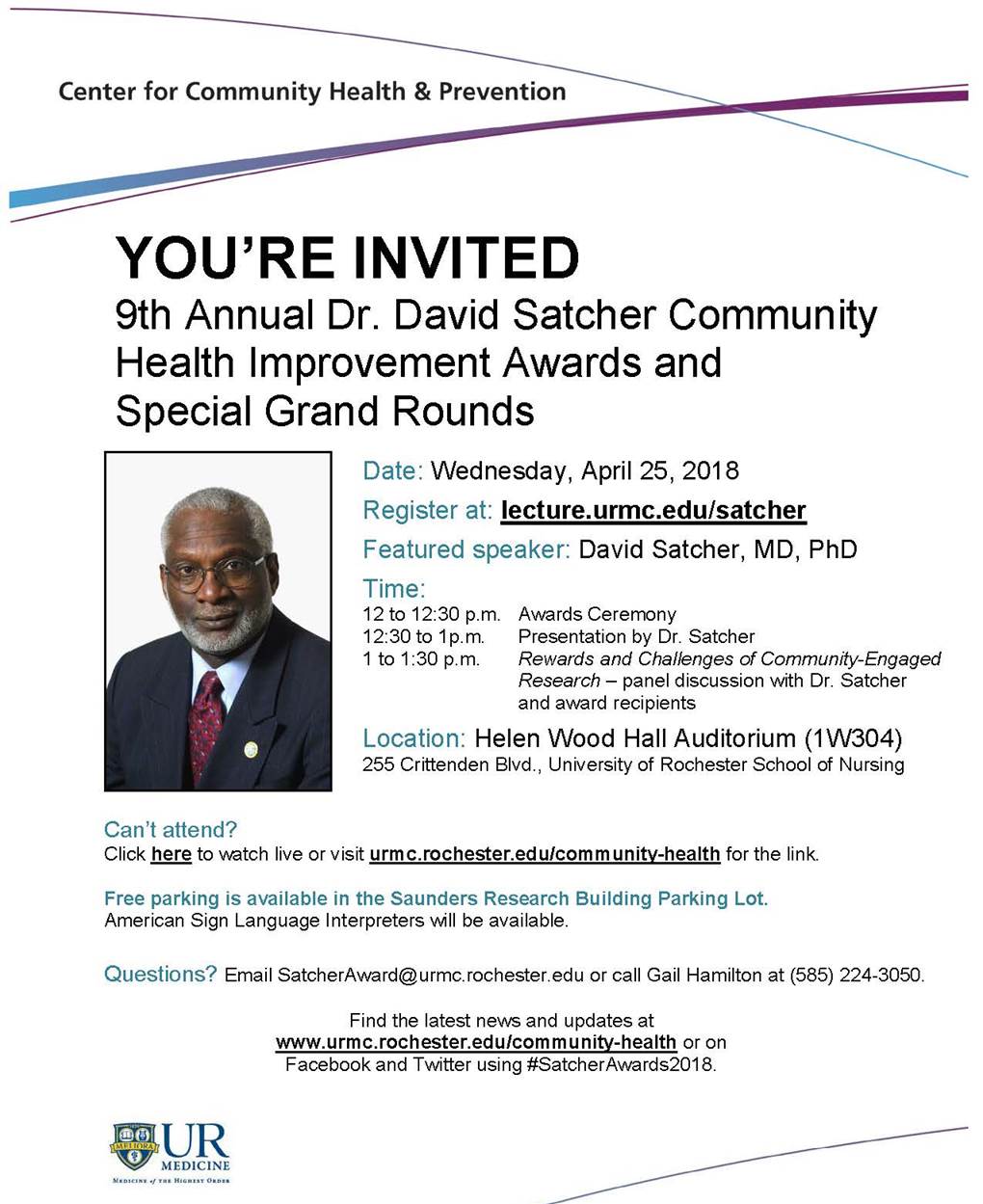
Satcher Awards 4/25
Keynote by David Satcher
The ninth annual Dr. David Satcher Community Health Improvement Awards and Special Grand Rounds features a keynote lecture by David Satcher ’72M (Res), the 16th Surgeon General of the United States.
The event runs from noon to 1:30 p.m. Wednesday, April 25, at URMC in the Helen Wood Hall Auditorium (1W304), School of Nursing.
Register online. Free parking is available in the Saunders Research Building parking lot. Direct questions to Gail Hamilton at 224-3050 or by email. ASL interpreters will be available, and the event can be viewed live online.
Drinking Too Much?
When to say when: Study says limit alcohol to 1 drink a day
This week several news outlets, including the Washington Post, reported that a new international study concludes there are “no overall health benefits from moderate drinking” and the “threshold for low-risk drinking … is about seven beers a week for men and women alike.”
The study was published on April 12 in The Lancet and was co-authored by 120 researchers based on “aggregated data from multiple studies of drinking patterns and health outcomes among nearly 600,000 people in 19 high-income countries.”
The Post says, “Strikingly, the data did not show a significant difference between men and women in the amount of alcohol that can be consumed without a drop in life expectancy” – a conclusion that contradicts US government guidelines.
USA Today reported that the US Office of Disease Prevention and Health Promotion’s guidelines “allow for drinking in moderation,” which, for men “means up to two drinks per day, or roughly 196 grams per week – nearly double what researchers suggest” in this study. For women, the guidelines say just “one drink per day, which is 98 grams per week.” Spain, Portugal, and Italy also have government recommended guidelines nearly 50 percent higher than the 100-gram threshold shown in this study.
The AP reported that the research “estimates that 40-year-old men who drink as much as the current U.S. guidelines allow can expect to live one to two years less than men who have no more than seven drinks per week.” The study found a “higher risk of stroke, heart failure, and other problems” among those who drink more than the study’s recommendation of about seven beers per week – or five glasses of wine or 1.5-ounce shots of liquor.
PBS NewsHour reported that the study suggests that “people who drank more than 100 grams of alcohol per week, the equivalent of about six glasses of wine, had increased risk of stroke, heart disease, heart failure, fatal hypertensive disease and fatal aortic aneurysm.”
What do you think?
Primary Care is Us
PCPs Are Becoming Rarer As Healthcare Business Models Change.
On the front of its Sunday business section yesterday the New York Times reported that “in this new medical age of urgent care centers and retail clinics… primary care” physicians are becoming “increasingly scarce.”
The article examined how changes in the healthcare industry have changed how patients receive medical care and interact with physicians.
Fortunately, our “business model” is growing and expanding to meet the complex needs of people who need and value more personal and comprehensive care that urgent care centers and retail clinics cannot and never will, by design, offer.
Do you or someone else you know need a primary care provider that really cares about you and your family? Just call us to set up an appointment. We look forward to serving you!
A dangerous weed
For psychiatric patients, a link between marijuana and violent behavior
Recreational drugs can wreak havoc on anyone’s life. But for those with mental illness, smoking pot could lead to aggressive behavior—and put their loved ones at risk.
According to a new study published in September in Frontiers in Psychiatry, adults who persistently smoke marijuana following a psychiatric hospitalization are 2½ times more likely to commit violent acts, including assault, battery, or threats with a weapon, than those who do not use the drug.
The study included 1,136 patients from ages 18 to 40 who received five follow-up appointments within a year after discharge from a psychiatric hospital. Not only did the researchers find that cannabis use put these patients at an increased risk for violent behavior, but they also discovered the risk is greater than for those using other mood-altering substances. “An interesting feature of our results is that the association between persistent cannabis use and violence is stronger than that associated with alcohol or cocaine,” Alexandre Dumais, the lead researcher, said in a statement.
The results support neuroimaging studies that show chronic marijuana users develop deficits in the prefrontal cortex, an area of the brain involved in inhibiting impulsive behavior, the researchers said. Problems with the prefrontal cortex have been correlated with antisocial personality and psychopathic traits.
The National Institute on Drug Abuse reviewed numerous studies on the adverse effects of cannabis use. They found that short-term effects may include impaired memory, decreased problem-solving ability, hallucinations, and delusions. Possible long-term effects include breathing problems, increased heart rate (which may raise the risk of a heart attack), onset or worsening symptoms of mental illness, depression, anxiety, and brain and behavioral problems for unborn and nursing babies whose mothers use the drug.
by Julie Borg in World Magazine
Teens starting with E-cigs?
E-Cigarettes May Create More Smokers Than Quitters, Research Suggests.
Bloomberg News (3/14, Wolf) reports that researchers at Dartmouth College’s Norris Cotton Cancer Center found that “vaping has led more people to start a real smoking habit, rather than avoid tobacco or quit in favor of e-cigarettes,” according to a study published Wednesday in PLOS One.
The researchers used census data, published literature, and surveys to build a model which showed that while 2,070 cigarette smokers in the US quit in 2015 with the help of e-cigarettes, 168,000 adolescents who had never smoked began smoking after first trying e-cigarettes. The authors suggested that “fruity flavors” have created a draw for younger users, and recommended that “should be the focus of restriction efforts by the” FDA.
Also reporting is HealthDay (3/14, Preidt).
Breast Feeding and Diabetes
The 30-Year CARDIA Study
Question
Is the protective association between lactation duration and progression to diabetes supported by a biochemical evidence basis?
Findings
Among young white and black women in this observational 30-year study, increasing lactation duration was associated with a strong, graded 25% to 47% relative reduction in the incidence of diabetes even after accounting for prepregnancy biochemical measures, clinical and demographic risk factors, gestational diabetes, lifestyle behaviors, and weight gain that prior studies did not address.
Meaning
This study provides evidence to support the hypothesis that lactation may lower risk of diabetes in women; these findings open new avenues into mechanisms leading to glucose intolerance.
As reported in a study by Gunderson, Lewis, Lin; et al in the January 2017 Journal of the American Medical Association (JAMA).
Herbal-Drug Interactions
Some Common Herbal Supplements May Have Dangerous Interactions With Common Prescription Drugs, Review Study Suggests.
TIME (1/24, MacMillan) reports some “common herbal supplements, including green tea and Ginkgo biloba, can interact with prescription medications” in “dangerous or deadly” ways, “according to a new research review published in the British Journal of Clinical Pharmacology.” Researchers reviewed “49 case reports of adverse drug reactions, along with two observational studies,” and concluded that herb-drug interactions were “highly probable” in 8% of the reports, “probable” in 51%, possible in 37%, and doubtful in 4%.
In one case report, a patient who took statins complained of intense leg cramps and pain—a commonly reported side effect—after drinking three cups of green tea a day. The reaction was attributed to green tea’s effects on statin levels in the blood, the researchers wrote, although they say more research is needed to rule out other possible causes.
In another report, a patient died after having a seizure while swimming, even though he was regularly taking anticonvulsant drugs for his condition. His autopsy, however, showed decreased levels of those drugs in his blood, likely due to the way Ginkgo biloba supplements—which he’d also been taking regularly—had affected their metabolism.
Taking herbal supplements has also been associated with worsening depression symptoms in people taking antidepressants, the authors wrote in their paper, and with organ rejection in those who had received kidney, heart or liver transplants. For cancer patients, chemotherapy drugs have been shown to interact with herbal supplements including ginseng, echinacea and chokeberry juice.
The analysis also showed that patients taking warfarin, a blood thinner, reported “clinically significant interactions” after taking herbal medicines containing sage, flaxseed, St. John’s wort, cranberry, goji juice and chamomilla. These herbs may affect the metabolism of warfarin, the researchers hypothesize, which may reduce its anticoagulation abilities or cause bleeding episodes.
Teens Smartphone Risk
Study Ties Sudden And Large Drop In Teen Happiness With Smartphone Proliferation.
The Washington Post (1/22, Bahrampour) reports researchers have tied “a sudden and large drop in adolescents’ happiness with the proliferation of smartphones and finding that the more hours a day teens spend in front of screens, the less satisfied they are.” Their report, called “Decreases in Psychological Well-Being Among American Adolescents After 2012 and Links to Screen Time During the Rise of Smartphone Technology,” was published online Jan. 22 in the journal Emotion. In arriving at their conclusions, the study authors analyzed data from “a large national survey of eighth, 10th and 12th graders conducted annually by the University of Michigan.” HealthDay (1/22, Preidt) also covers the study.










 I'm a happy person who loves getting to know and being able to help people of all ages. I connect with little children (and the little child in most adults) almost immediately. Sharing the joys and trials of relationships, pregnancy and delivery, and family life are the things about family practice that really light my fire. I've found that having a sense of humor and seeing God's love at work can see us through some of life's most difficult times, if we can keep the faith and hang in there together.
I'm a happy person who loves getting to know and being able to help people of all ages. I connect with little children (and the little child in most adults) almost immediately. Sharing the joys and trials of relationships, pregnancy and delivery, and family life are the things about family practice that really light my fire. I've found that having a sense of humor and seeing God's love at work can see us through some of life's most difficult times, if we can keep the faith and hang in there together. 


