Celebrating success
CMMI program celebrated
The success of FLHSA’s Centers for Medicare and Medicaid Innovation (CMMI) award was highlighted during a celebration with staff and members of the Rochester Health Innovation Collaborative in November. The initiative in 65 primary care practices showed a 50-percent drop in hospital admissions and a 40-percent drop in emergency room visits for people who received care management.
His Branches Health Services was an active part of the CMMI project for the past 2+ years and has been extremely grateful for the support and training we have received. Click here to learn more about the demonstration project.
From left, New York State Assembly Majority Leader Joseph Morelle, CEO Trilby de Jung and Chief Medical Officer Dr. Thomas Mahoney
Penalize doctors?
Moving Toward Outcome Measures
by Leigh Page
As physician payment begins to shift to value-based payments, the measures of quality care will slowly move from processes to outcomes.
That’s a relief for some doctors who have never liked reporting process measures and instead wanted to be judged by their outcomes. But outcomes also present a new burden: Doctors will be held accountable for patients who don’t improve because they aren’t following the treatment plan they recommended.
“Most doctors don’t mind being judged on their quality of care,” says Kevin Campbell, MD, a cardiologist at the University of North Carolina. “But if the physician has done everything right for the patient and the patient is non-adherent, should that reflect poorly on the clinician?”
The answer from some adherence experts is “yes,” although that answer is disputed by many physicians. Assuring patients’ adherence is as much a part of being a good doctor as drawing up a successful treatment plan, says Stephen Wilkins, MPH, a former hospital executive who runs Mind The Gap Academy, a San Jose, California, group that seeks to improve outcomes through better physician/patient engagement.
Even when patients decide not to follow the treatment plan, Wilkins thinks physicians should bear some financial responsibility for the resultant poor outcome. “Physicians should be checking prescription fill and refill rates, or taking similar measures,” he says.
Many physicians have strong feelings against this type of sentiment. Their view is that patients should bear a large degree of responsibility for their own health and health-related decisions. Why should a doctor pay the price if a patient continues to drink too much, continue smoking, or gorge on french fries? Others, though, feel that with today’s apps and electronic communications, it has become less burdensome for doctors to urge patients toward better outcomes.
Click here to read the entire article, published in Medscape on November 3, 2016.
GNOC Banquet
A Town and Gown Celebration
Thursday evening a group of us who serve at Joy Family Medicine scooted out of the office in time to fill a table of 8 at the first annual Gerhardt Neighborhood Outreach Center (GNOC) Banquet.
Dr. Morehouse and Susan were joined at the elegant Shadow Lake event by Ali and Greg Reeves, April, Gloria, Jen, and Susan Kerr for a dress-up evening of dinner and great jazz entertainment with Alvin Parris and band where we learned more about the GNOC and heard some wonderfully encouraging testimonies.
At the end of the evening an award was presented for “Outstanding Service to the Community.” As the award was being described we were all wondering who, of the many people in attendance, might be receiving it. Imagine our surprise when Dr. Morehouse and Susan were called up front and honored! Hey, you never know!
An interesting mystery
Study Suggests Placebo Benefits
CNN (10/27, Scutti) reports that findings from “a new study published in…Pain suggest that a placebo can have real, even profound, physical benefits.” The study’s participants, all of whom had chronic lower back pain, were divided into two groups, one of which continued to receive nonsteroidal anti-inflammatory medications, and another that “received their usual pain drugs as well as placebo pills in a typical prescription medicine bottle.” These participants “were told that a placebo pill contained no medication, and the bottle’s label read ‘Placebo pills. Take 2 pills twice a day.’”
The NPR (10/27, Hobson) “Shots” blog reports that the investigators “found that people who received the placebo saw their scores for both usual and maximum pain levels drop by 30 percent, compared to 9 percent and 16 percent declines for the control group.” Additionally, “the placebo group…reported a 29 percent reduction in their score for difficulty in performing daily activities, while the control group saw no change.”
Comment:
What is not discussed in the study is how long the beneficial effects lasted. Initial improvement is a common finding when people first start taking any of a number of different supplement and homeopathic remedies that have been recommended to them: after an initial phase of symptom relief, the apparent daily effectiveness wears off as the weeks go by and is usually gone within months.
Heart Failure Risk
NSAIDs Increase Heart Failure Risk
A research study recently published in the British Medical Journal found that people who used some commonly used non-steroidal anti-inflammatory drugs (NSAIDs, see list below) had a 19% higher risk of hospital admission for heart failure overall. The study further found that the rate was much higher for Toradol (ketorolac – 83%), than for Aleve (naproxen – 16%), and some such as Celebrex (celecoxib) were associated with little or no increased risk.
In an accompanying editorial, Dr. Gunnar H. Gislason, chief scientific officer of the Danish Heart Foundation, wrote, “There is difference between the NSAIDs in risk of heart failure and higher dosages are associated with increased risk.” He concludes that the study shows “the elderly and patients with any heart condition should avoid NSAIDs.” The study was based on data covering 92,000 people admitted to hospitals in the Netherlands, Italy, Germany and the U.K. from 1999 to 2010.
Click here for a fairly comprehensive list of NSAIDs. Note that at least two of these (Vioxx and Bextra) have been removed from the market and that OTC products like aspirin taken in low doses were not clearly identified as a risk.
Churches can help
A new video
shows how Rochester churches have inspired members to eat healthier, get active and lower their blood pressure. The three-minute story follows the work of the Interdenominational Health Ministry Coalition, a group of volunteer health champions who partner with the High Blood Pressure Collaborative in more than 20 churches.
Produced for the Collaborative’s Urban Wellness Summit at the Maplewood YMCA held on September 29, the video includes participants sharing their motivations for lifestyle change, like this father’s love for his two-year old son: “I want to make sure that I’m around to see him grow up.”
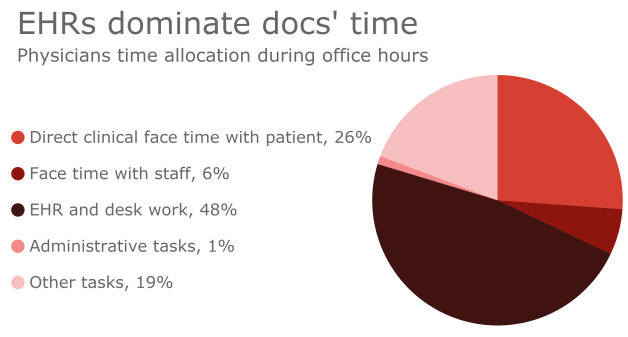
EHR devours MD time
A new AMA-supported study found that physicians spend far more time working on electronic health records (EHRs) and desk work than they do meeting face to face with their patients. Published online Sept. 6 by Annals of Internal Medicine, the study, “Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties,” involved observations of 57 U.S. physicians in family medicine, internal medicine, cardiology, and orthopedics who were observed for a total of 430 hours, with 21 of them also completing after-hours diaries.
Click here to read the study summary and here for a link to the original study.
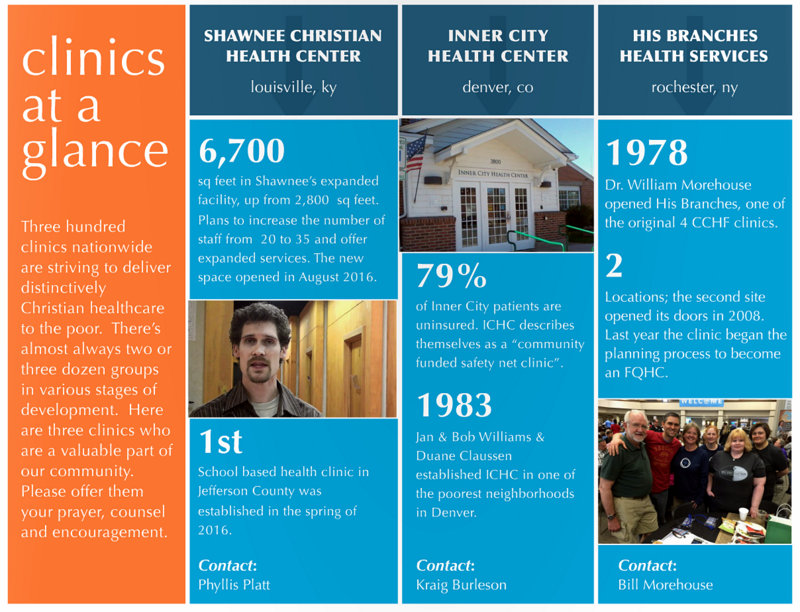
CCHF Highlights HBHS
Summer Newsletter 2016
Check out this summer’s edition of the CCHF newsletter, just out August 26, for a cameo appearance of our ministry!
Six of us attended the annual CCHF Conference this year in Oklahoma City and were energized by the fellowship, teaching, and worship we experienced together. For over 30 years CCHF has been an inspiration to us and centers serving the underprivileged like ours around the country. It’s an honor to have them standing with us in prayer and support for the future of our ministry.
Read the newsletter in flipbook format above, or download a PDF version.
NHSC Opportunities
New NHSC Poster Available!
The NHSC has created a new poster to highlight its scholarship and loan repayment programs for potential applicants.
Please feel free to display the poster in various settings to raise awareness about available opportunities to primary health care students and practicing clinicians.
We also encourage you to share the poster with relevant networks through your outreach channels.
Thank you.
National Health Service Corps

- Students pursuing primary care careers: The Scholarship Program pays for tuition and fees of future primary care providers, including physicians, dentists, nurse practitioners, certified nurse midwives, and physician assistants.
- Primary care providers interested in serving communities in need: The Loan Repayment Program provides up to $50,000 for loans in primary care—medical, dental, or mental/behavioral health.
- Students in the final year of medical or dental school pursuing primary care careers: The Students to Service Program provides up to $120,000 to students pursuing degrees in primary care and are in their final year of medical or dental school.
FQHC Application is in!
After 3 months of prodigious work
by our dedicated Federally Qualified Health Center (FQHC) application team, led by Stephanie Smith with expert assistance from Jan Thirlby, Deb Blanchard, Valerie, Norm, Josh Moody, and many more staff and Board members, we’ve finally succeeded in submitting our full application for FQHC New Access Point (NAP) designation!
This was truly the “heavy lift” we had anticipated, and even more! The huge page Phase 2 application, which was due on July 15, had our teams meeting daily as we drew closer to the deadline and nearly overnight for the last two days. We strengthened our Board by adding 3 new members, added final tweaks to our Policies & Procedures Manual, solicited and received over 2 dozen very encouraging letters of support from churches, community groups, health care organizations, and governmental officials, wrote reams of analysis, planning, and implementation narrative, and gathered information about budget, position descriptions, and staff biographical sketches.
Please pray for the HRSA reviewers as they consider our full NAP application in the weeks ahead and for our team as they regather later in this year to revisit the materials we’ve submitted and reshape them into a backup FQHC “Look-Alike” application for submission.











 I'm a happy person who loves getting to know and being able to help people of all ages. I connect with little children (and the little child in most adults) almost immediately. Sharing the joys and trials of relationships, pregnancy and delivery, and family life are the things about family practice that really light my fire. I've found that having a sense of humor and seeing God's love at work can see us through some of life's most difficult times, if we can keep the faith and hang in there together.
I'm a happy person who loves getting to know and being able to help people of all ages. I connect with little children (and the little child in most adults) almost immediately. Sharing the joys and trials of relationships, pregnancy and delivery, and family life are the things about family practice that really light my fire. I've found that having a sense of humor and seeing God's love at work can see us through some of life's most difficult times, if we can keep the faith and hang in there together. 


